Caring for wounds at home can be challenging for patients, caregivers and loved ones. A typical form of wound care at home is caring for a patient after a surgical procedure. The National Institutes of Health (NIH), reports that over 11% of Americans undergo surgery each year. Nearly 20% of these patients are over the age of 65. Wound care at home impacts patients, caregivers and loved ones. Caring for patients recovering from a wound takes time, patience and skill. Chronic wounds affect over 6.5 million adults in the U.S. annually, according to the American Academy of Homecare Medicine.
Typically, seniors in particular may present a greater challenge to caregivers because healing from a wound takes longer as one ages. This article will help you learn about different wound types and essential care tips. Additionally, it will help you find the right wound care products at Honest Medical.
Acute vs. Chronic Wounds
Generally, wounds can be classified as either acute or chronic in nature:
| Acute Wounds | Chronic Wounds |
|---|---|
| These are wounds that progress through the normal stages of wound recovery and show signs of healing within four weeks. | This type of wound does not progress through normal healing stages but becomes stalled or otherwise does not show signs of healing within a four-week period. |
Types of Wounds
Within the major categories of acute and chronic wounds, there are different types of wounds including the following:
| Type of Wound | Description |
|---|---|
| Abrasions | Superficial wounds to the skin where the epidermis or surface layer of the skin is penetrated are called abrasion wounds. These wounds can be caused by scraping, brushing, impact, friction or pressure. Typical abrasions are skinned knees from a fall or scraping the skin against a sharp edge. Abrasions can be minor to severe depending on how much of the skin is involved. |
| Lacerations | Anytime tearing of soft body tissue occurs, there is a laceration. Lacerations are often jagged and irregular. They can be caused by any sharp object and are vulnerable to infection from any bacteria that may be on the object causing the wound. |
| Burns | These wounds are classified by the depth and severity of the damage to the skin. There are degrees of burns one through four. For comprehensive burn wound care guidance, check out our blog post, “Essential Steps for Burn Wound Care” |
| Surgical Incisions | Surgical incisions are precisely made to access internal structures. Their size depends on the procedure’s requirements. |
| Pressure Injuries | These wounds are often referred to as pressure sores, bedsores or ulcers. They occur when pressure cuts off blood circulation to some part of the skin. Bedsores, a type of pressure injury, form when skin is compressed against bone for extended periods due to immobility. This lack of blood flow can cause tissue breakdown, leading to painful sores in areas like the heels, shoulders, elbows, sacrum, and back of the head. |
| Ulcers | When a wound becomes ulcerated, it forms an open sore that can ooze clear fluid, pus or blood. These wounds can be very painful and sometimes infected, and they won’t heal without proper care. Ulcers can develop from pressure wounds or infected cuts and can be very hard to heal. If not treated, ulcers can lead to deeper infections involving bone and blood. |

Wound Care at Home
Caring for wounds at home can include a range of wound types. You can review the following tips and best practices for wound care at home. Included are links to products that can make wound care at home easier for patients, caregivers and loved ones.
🩹 Minor Wound Care
Minor wounds are cuts or scrapes that break the skin, but generally don’t require professional treatment such as stitches.
- First, stop the bleeding: Use a clean cloth or gauze to apply gentle pressure to the wound to stop the bleeding. Don’t ignore severe bleeding or deep wounds. Seek professional care to determine if stitches are necessary.
- Clean the wound: Use saline solution or a mild wound cleanser to remove any dirt and debris from the wound. Use a mild soap to wash the wound before rinsing and drying it thoroughly. If the wound contains foreign objects such as glass or gravel, a healthcare professional should examine it.
- Use a topical antibiotic: Apply a thin layer of antibiotic ointment to the wound to prevent infection before applying a dressing.
- Dress and bandage the wound: Cover the clean wound with a dressing to facilitate healing. Use waterproof bandages and gauze to make sure the wound stays clean as it heals.
- Change the dressing: It is important to change the dressing on wounds with clean gauze and adhesive bandages on a regular basis. Healthcare professionals recommend changing dressing and bandages, and checking the wound for infection every 24 hours. Make sure the wound stays dry as it heals.
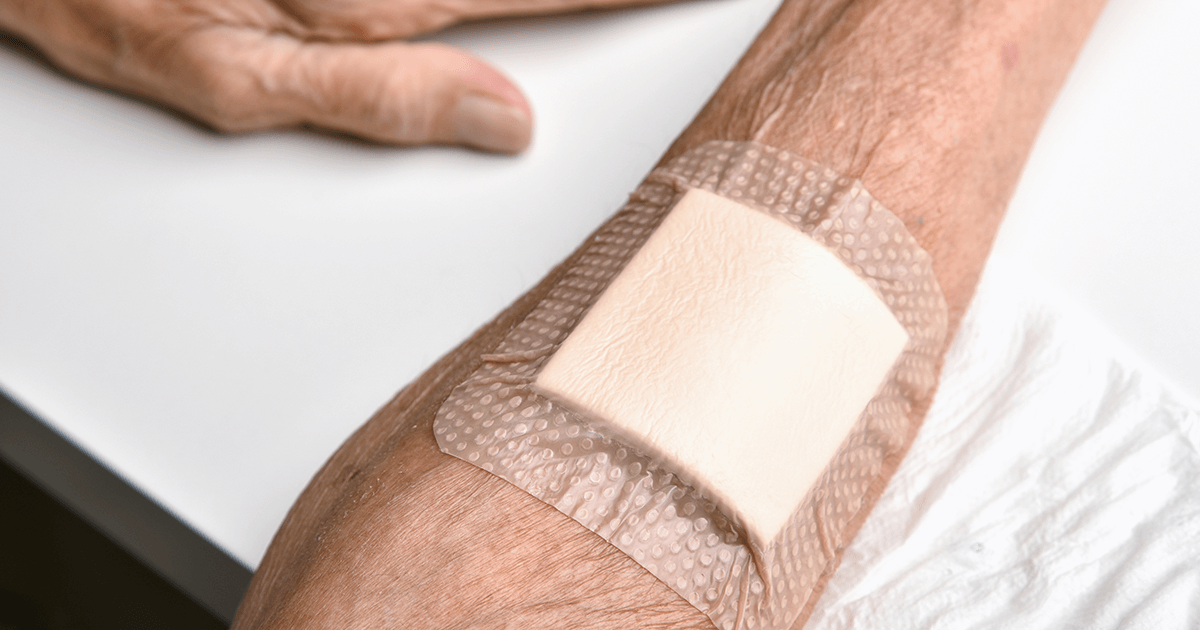
🩹 Surgical Wound Care
After surgery, take charge of your recovery with proper wound care. Follow your doctor’s advice and consider these additional tips.
- Keep the wound clean: This means thoroughly washing your hands before cleaning the wound and wearing gloves. If your surgeon approves, you can clean the skin around the incision using mild soap and water or saline solution. However, you should avoid using harsh cleansers such as alcohol, iodine or antibacterial soap as they can harm the skin around the incision site. Use a soft cloth or gauze pad and clean the skin gently. Make sure to dry the skin or let it air dry before applying a clean dressing. Dispose of the old dressing and put on new gloves.
- Inspect the wound for infection: A surgical wound should be inspected frequently for signs of infection. Typically, redness and swelling can be signs of infection but these may also be a normal part of healing if they occur within a few days after the surgery. If you continue to have redness, swelling, pus coming from the incision, or you are experiencing a fever, chills or general feelings of illness, you should contact your doctor.
- Apply a new dressing: Your doctor or nurse can tell you what type of dressing to use, though typically sterile soft gauze pads are ideal, particularly if there is fluid drainage. Your doctor could suggest a waterproof dressing, so you can bathe with your incision protected, but be sure to follow whatever directions you receive.
- Tape the dressing: Your doctor will tell you at what point the wound can be left uncovered to heal in the open. If tape must be applied, you should cover the gauze completely with waterproof tape.
- Take showers not baths: Showers are recommended after surgery to avoid soaking in a bath, which can risk exposing the surgical wound to bacteria. Be sure to completely cover the wound with the sterile dressing before applying waterproof tape.
- Protect the incision as it heals: Once the incision is fully exposed and healing, you should avoid exposing it to the sun for at least six months after the surgery. A sunburn can increase scarring, so if you must be outside, make sure you use sunscreen or cover the scar with tape.
- Eat well, rest and avoid intense exercise: As you heal from surgery, it’s important to reserve your strength and avoid heavy lifting or intense workouts that can compromise healing. Be sure to drink plenty of water and eat a healthy diet to ensure you get the best outcomes from your recovery. Seniors recovering from surgery may not have much of an appetite. Adding nutrient-dense supplements such as ensure will help boost their recovery during these early stages as they heal.
🩹 Chronic Wound Care
Seniors often face the challenge of chronic wounds, such as pressure ulcers, which can be slow to heal. While your healthcare provider’s guidance is essential, you can also implement these best practices for effective home wound care.
In general, chronic wounds are wounds that take longer than four weeks to heal. The following are some tips for caring for chronic wounds at home.
- Take the medications your doctor prescribes: You may be prescribed pain killers, or antibiotics to deal with your chronic wound. Be sure to take your medications exactly as prescribed and especially in the case of antibiotics – take the full course without skipping any doses. If you are diabetic be sure to keep up with the medication for treating your diabetes as this disease can slow the healing process.
- Clean the wound: As with any wound – make sure your hands are clean and wear gloves. After you dispose of a used dressing, put on a new pair of gloves. Initial cleansing and debridement of chronic wounds are typically done by a health professional. If your doctor feels the dressing can be changed at home, follow the instructions carefully. In most cases, the wound should be cleaned using a saline solution. If it looks like there is dead skin or other matter building up, ask your healthcare professional before proceeding.
- Change dressings: Typically, dressings are left on chronic wounds for a longer period of time so that any discharge can be absorbed by the dressing. Your healthcare professional can tell you what type of dressing is appropriate. The following types of dressings are often used to soak up excess fluid: film dressing with pads, gauze, hydrogel dressing, hydrocolloid dressing, alginate dressings or foam dressings. Change the dressing when it looks like it’s reached capacity for soaking up leakage from the wound.
- Keep pressure off the wound: Make sure no pressure is applied to the wound and keep clothing around the wound as loose as possible. If you have a bedsore, or are in danger of developing one, elevate the affected area to take pressure off it. Also, turn in your bed every two hours and use wedges and pillows to change position and pad areas where pressure is occurring.
- Exercise when possible: Under the direction of your doctor, exercise can help increase blood flow and speed healing. If you feel up to it, moving around or doing light exercise sessions on a regular basis can improve overall health as well as help you heal.
- Eat healthy and stay hydrated: As with any healing process, eating a nutrient-rich diet filled with fresh fruit and vegetables and healthy proteins is important for the healing process. It is also vital to drink plenty of water and avoid alcohol, which can slow healing.
Honest Medical Has the Wound Care Products You Need
Wound care at home takes time and patience for both patients and caregivers. However, it’s important to follow your doctor’s directions as well as having the right products to keep wounds clean. Our diverse range of wound care products caters to both acute and chronic wounds. Visit our site and browse through thousands of health and wellness products. You can also speak to an Honest Medical Care Specialist at (833) 933-2323. We’re here to provide you with product knowledge, support, and expertise to ensure you get the right products for your unique needs and budget. Check out our other published articles on caregiving and more!




I need some assistance with recurring staph infections
Dear Kathryn,
Thank you for reaching out to us with your concern about recurring staph infections. We understand that this can be a challenging issue to deal with. While we can’t provide medical advice, we can offer some general information that may be helpful. It’s important to consult with a healthcare professional for a proper diagnosis and treatment plan.
Here are some best practices that can help prevent staph infections:
You can find more general information from online sources like Mayo Clinic here https://www.mayoclinic.org/diseases-conditions/staph-infections/symptoms-causes/syc-20356221 but we recommend speaking to your primary healthcare provider for a personalized treatment.
Hope this helps!